How To Choose the Best Probiotic Suppositories
Lactobacillus acidophilus is the most researched probiotic strain for maintaining vaginal balance [10]. Two other key strains, Lactobacillus rhamnosus and Lactobacillus reuteri, help by sticking to vaginal surfaces and preventing harmful bacteria from growing. They may also bind to bad bacteria, stopping them from spreading, and restore a healthy microbiome [12].
When selecting from Lactobacillus suppositories, look for the right ingredients to support your vaginal health. Lactobacillus crispatus is a powerhouse for preventing BV and keeping your vaginal microbiome balanced [13]. Lactobacillus reuteri and Lactobacillus rhamnosus are also great for both BV and yeast infections, helping replenish good bacteria [12]. If you struggle with chronic BV or recurring yeast infections, a boric acid and probiotic suppositories combo can offer extra relief and protection [14], [15].
You’ll also want to consider a pH-balanced formula, which helps maintain the ideal environment for good bacteria to thrive [1]. Some suppositories are meant for daily maintenance, while others are designed for short-term recovery. Certain products even include prebiotics, vitamin C, or boric acid for an added boost [15-17].
Just as important as what’s in your suppository is what’s not in it. Stay away from artificial fragrances and preservatives, which can lead to irritation, and avoid harsh chemicals that could throw off your vaginal flora [18]. The right probiotic suppository can help restore balance, keep infections at bay, and support overall vaginal health — so choose wisely.
How To Use Probiotic Suppositories
Once you’ve picked the right suppository, here are some dosage and application tips for easy reference.
BV Treatment: One suppository daily for 7 days after antibiotics [19]
Yeast Infection Prevention: Twice per week [20]
Vaginal Health Maintenance: One to two times per week [21]
When NOT to Use:
- Don't use this treatment during an active yeast infection — start with an antifungal first [6].
- If BV symptoms are severe, antibiotics may be needed before probiotics [5].
- Always consult a doctor before using this treatment during pregnancy [22].
If you still need some help deciding, here’s a side-by-side comparison of probiotics in suppository versus oral form to give you a clearer picture.
Probiotic Suppositories vs. Oral Probiotics: Which Is Better?
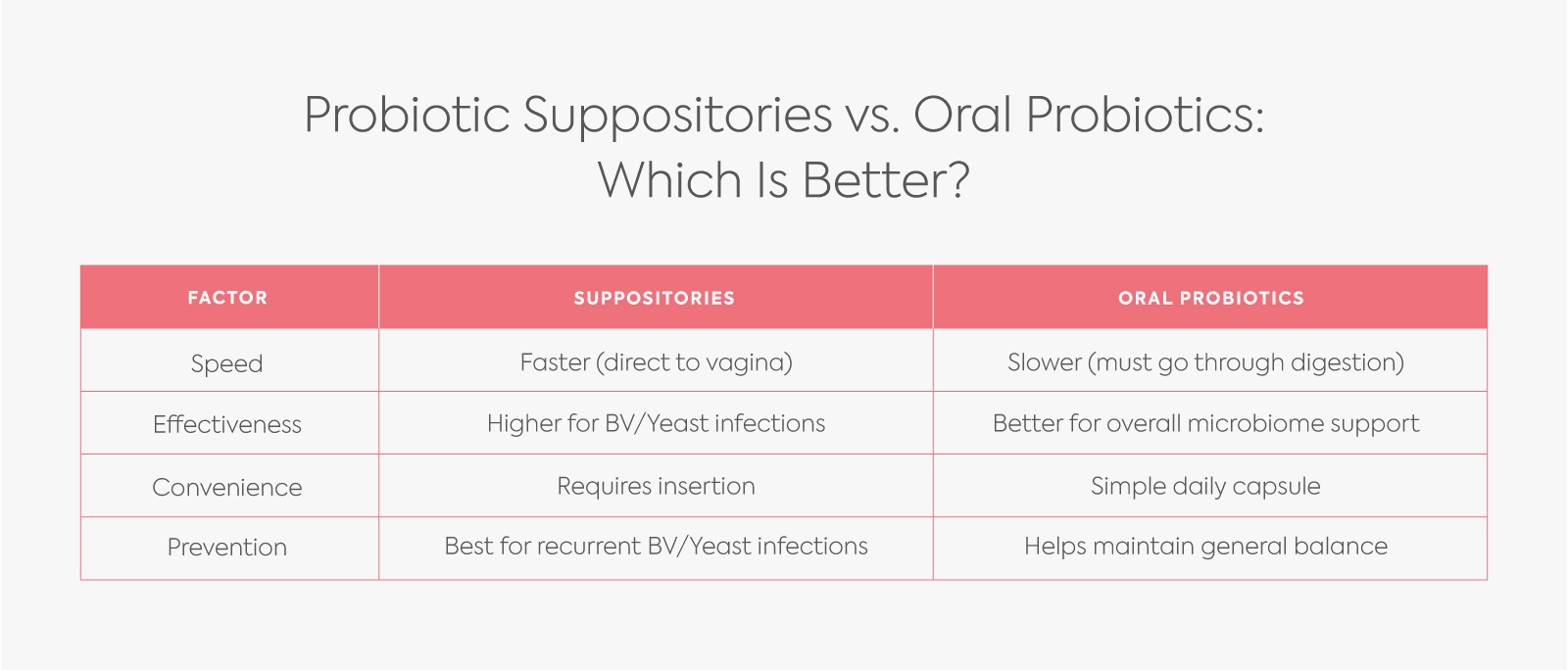
Probiotic suppositories and oral probiotics both help support vaginal and overall microbiome health, but they work in different ways. Suppositories are inserted directly into the vagina, making them a faster option for treating bacterial vaginosis (BV) and yeast infections. They are considered more effective for these specific infections because they deliver probiotics directly to the affected area. However, they require insertion, which may be less convenient for some people. Suppositories are especially beneficial for recurring BV or yeast infections since they help restore vaginal flora more quickly.
Oral probiotics, on the other hand, must go through digestion, so they work more slowly but provide overall microbiome support. Taking a simple daily capsule is more convenient than using a suppository, and oral probiotics are ideal for maintaining long-term vaginal balance rather than treating active infections. Choosing between the two depends on individual needs—suppositories are better for immediate relief from infections, while oral probiotics are great for overall gut and vaginal health maintenance.
Probiotic Suppositories for BV, Yeast Infections, and Pregnancy
For Bacterial Vaginosis:
Probiotic suppositories work best after completing antibiotic treatment to help prevent recurrence. Using a Lactobacillus-based formula can restore pH balance and support a healthier vaginal microbiome, making it harder for harmful bacteria to thrive [9], [25].
For Yeast Infections:
Probiotics can help restore balance after antifungal treatment. Strains like Lactobacillus reuteri and Lactobacillus rhamnosus are particularly beneficial in keeping yeast levels in check and preventing future infections[9,25].
During Pregnancy:
Probiotic suppositories are generally considered safe, but it’s always best to check with your doctor before use [7]. Avoid products containing boric acid, as it may not be safe for pregnancy [14]. Opt for gentle, Lactobacillus-based options to support vaginal health without unnecessary risks [22].
Key Takeaways and Practical Advice
For the best results, use probiotic suppositories after finishing antibiotics or antifungals, not during an active infection. Choose a Lactobacillus-based formula to restore balance, as oral probiotics aren’t as effective for BV or yeast infections.
If you struggle with recurring infections, a probiotic and boric acid combo may help prevent them. To stay on top of your vaginal health, consider testing your vaginal pH regularly with Diagnox’s Vaginox. This kit can help you spot imbalances early and take action before issues arise.







.webp)





